Icare Finland. Icare TA01I tonometer [Internet]. 2017 [cited 2017 May 17]. Available from: https://youtu.be/YPtDxGmQpFQ
Glaucoma Visual Field Progression and Intraocular Pressure (IOP) Measurements
For those with glaucoma, higher intraocular pressure (IOP) is associated with faster vision loss. There are now multiple different types of tonometry used to check IOP. It’s reasonable, then, to ask, “Is any one of these methods of checking IOP better at monitoring glaucoma?”
Is any one of these methods of checking IOP better at monitoring glaucoma?
Bianca Susanna and colleagues at the University of California, San Diego addressed this question at the recent American Glaucoma Society (AGS) 2017 Annual Meeting in Coronado, CA (March 2-5) in a paper entitled “Association Between Rates of Glaucoma Visual Field Progression and Intraocular Pressure (IOP) Measurements Obtained by Different Tonometers”.
However, one method of tonometry stood out as superior.
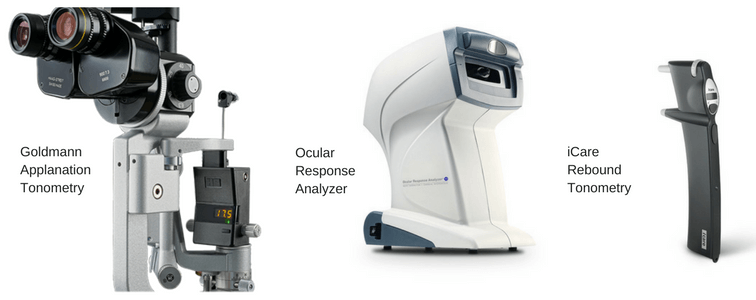
Photo Credit: Goldmann Applanation Tonometry: www.haag-streit.com | Ocular Response Analyzer: www.reichert.com | Icare Rebound Tonometry: /www.icaretonometer.com
This study compared the readings of three types of instruments against visual field loss in patients with glaucoma. The instruments used were:
- Goldmann applanation tonometry (GAT) which is commonly considered to be the “gold standard” of IOP measurement
- iCare rebound tonometry (RBT) which is both portable and used by the majority of glaucoma patients who perform home-based IOP measurements.
- Ocular Response Analyzer (ORA) which provides a corneal-compensated IOP (IOPcc)
213 eyes of 125 glaucoma patients were followed for an average of roughly two and a half years. At each visit the IOP was measured using each of the above three devices. Visual field progression was assessed using standard automated perimetry (SAP). The Ocular Response Analyzer tended to measure a bit over 1mmHg higher than GAT which on average measured 1mmHg higher than the iCare rebound tonometer. Not surprisingly, higher IOP measurements with any of the three devices were associated with faster visual field loss.
However, one method of tonometry stood out as superior. Measurements from the Ocular Response Analyzer had the highest correlation (relationship) with visual field loss over time. In other words, higher IOPcc as measured with the Ocular Response Analyzer was more predictive of eventual visual field loss than measurements from either GAT or iCare rebound tonometry.
Why would this be?
Corneal properties are known to affect the measurement of IOP.[1] Indeed, the biomechanical properties of the corneal may well have a relationship with glaucoma that extends beyond just IOP measurement.[2] One property in particular, corneal hysteresis, is known to be correlated with glaucoma risk. The Ocular Response Analyzer measures corneal hysteresis and uses this to “compensate”(adjust) the IOP measurement. This compensation is not done with either standard Goldmann applanation tonometry or iCare rebound tonometry (RBT).
The results of this study provide a rather compelling reason to measure corneal hysteresis as well as IOP in patients with glaucoma. Despite this, I would not expect to see Ocular Response Analyzers in most eye care practices anytime soon. A few reasons for this include:
- It will take far more than a single paper presented at a glaucoma conference (even a well-attended one) showing a slight improvement in predictive ability of IOPcc over IOP to topple the long-held belief that Goldmann applanation tonometry is the “gold standard”.
- Every ophthalmologist’s office already has one or more Goldmann applanation tonometers. They are relatively inexpensive (approximately $2,000), low maintenance, mechanical (no electronic components to degrade), reliable, and last for decades.
- The Ocular Response Analyzer is an expensive (just under $20,000), technologically complex (likely to get “buggy” over time as do all electronic devices), and though it may last for a decade or so only comes with a 1-2 year warranty (placing the purchasing doctor at significant financial risk if it breaks down). Additionally, there is really no practical method for the doctor to cover this financial risk. Although there is a billing code for corneal hysteresis (CPT 92145) it only “allows” for about $16 per test and is, in reality, seldom paid by insurances or Medicare.
I am hopeful that additional research will be done to further support the role corneal hysteresis testing in the ongoing assessment of glaucoma. Perhaps this will encourage other manufacturers to develop their own corneal hysteresis measuring devices. With competition in the marketplace the price of this technology might drop to a level that would allow more eye doctors to justify investing in this technology further benefiting their patients at risk of loss of vision from glaucoma.
Reference:
[1] Kotecha A. What biomechanical properties of the cornea are relevant for the clinician? Surv Ophthalmol. 2007;52(Suppl 2):S109-14.
[2] Medeiros FA, Meira-Freitas D, Lisboa R, Kuang TM, Zangwill LM, Weinreb RN. Corneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal study. Ophthalmology. 2013;120:1533-40.
Don’t delay getting checked for glaucoma
Make an appointment with an eye doctor in your area now. If you live in the greater Los Angeles area and would like Dr. David Richardson to evaluate your eyes for glaucoma call 626-289-7856 now. Appointments are available Tuesday through Saturday.

David Richardson, MD
Medical Director, San Marino Eye
David Richardson, M.D. is recognized as one of the top cataract and glaucoma surgeons in the US and is among an elite group of glaucoma surgeons in the country performing the highly specialized canaloplasty procedure. Morever, Dr. Richardson is one of only a few surgeons in the greater Los Angeles area that performs MicroPulse P3™ "Cyclophotocoagulation" (MP3) glaucoma laser surgery. Dr. Richardson graduated Magna Cum Laude from the University of Southern California and earned his Medical Degree from Harvard Medical School. He completed his ophthalmology residency at the LAC+USC Medical Center/ Doheny Eye Institute. Dr. Richardson is also an Ambassador of Glaucoma Research Foundation.


