Canaloplasty After Failed Trabeculectomy
Given the technical difficulty of canaloplasty combined with unpredictable insurance coverage, it is no surprise that canaloplasty is rarely the “first-line” or primary choice of glaucoma surgeons. As such, trabeculectomy is often the first glaucoma surgery performed on those whose intraocular pressures (IOP) are not well controlled with drops alone. Of those who have had trabeculectomy, however, almost half will require additional glaucoma surgery in as little as five years. [1]
Indeed, almost half of those who have repeat trabeculectomy may experience loss of IOP control in only three years (compared to five years with primary trabeculectomy)
What, then?
Traditionally, a “failed” trabeculectomy is treated by either a second trabeculectomy or by placement of a glaucoma drainage device (”tube”). Both of these options carry significant risk of post-op complications: as many as one third of all patients who elect to have a “trab” or “tube” may experience a complication after surgery.[2] That’s not even all the bad news: for those who choose repeat trabeculectomy the risk of failure to control IOP is even higher.[3]
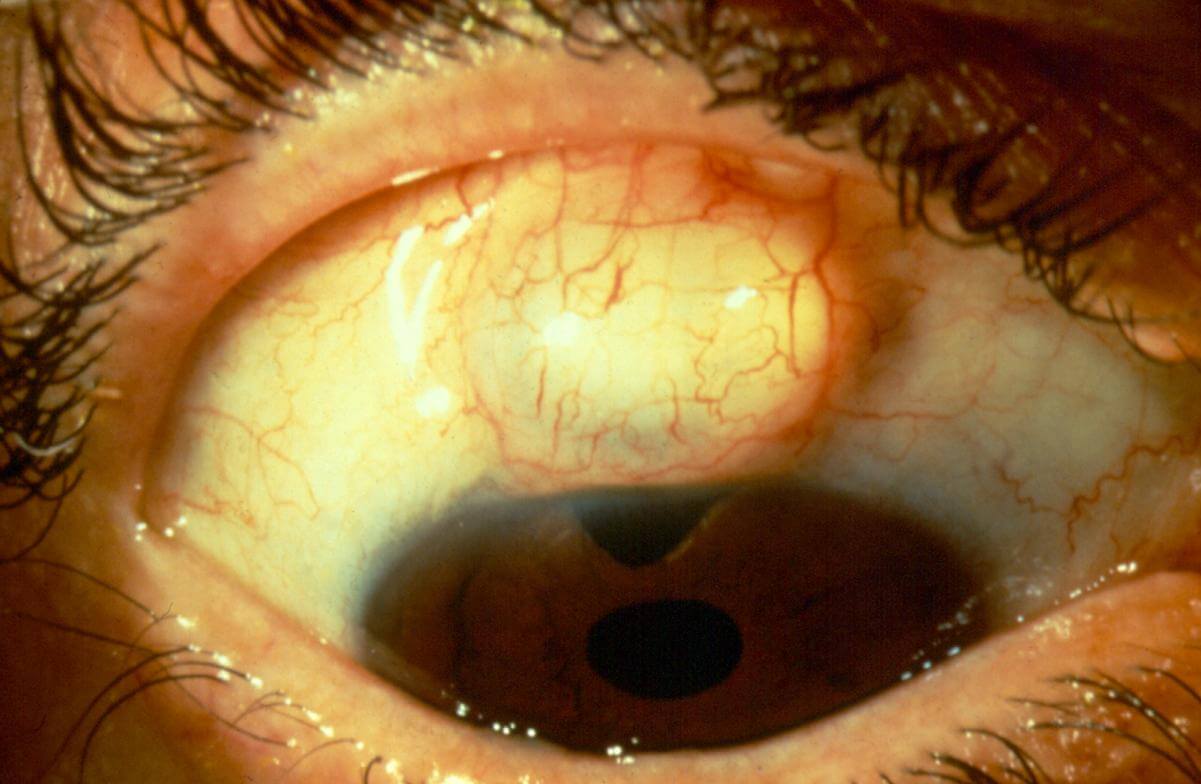
Photos 1,2: Photos of Bleb | Photos 3,4: Published Studies on Efficacy of Canaloplasty After Trabeculectomy
Indeed, almost half of those who have repeat trabeculectomy may experience loss of IOP control in only three years (compared to five years with primary trabeculectomy).
Not All Trabeculectomies Are The Same
If, during the creation of a trabeculectomy, Schlemm’s canal is undamaged then canaloplasty may be performed with little added risk or complication compared to primary canaloplasty. In such cases canaloplasty can successfully lower IOP after failed trabeculectomy.[4] Unfortunately, many trabeculectomies result in damage to the canal. When the canal is damaged, the canaloplasty catheter cannot fully encircle the canal. Full catheterization is required in order to stent open the canal. As such, it had been thought that canaloplasty with full catheterization of the canal could not be done unless the canal was fully patent (without obstruction, loss, or scarring).
This technique, “Relay Suture Guided Canaloplasty” (ReSGu Canaloplasty), is more challenging than primary canaloplasty.
ReSGu Canaloplasty to the Rescue
In late 2016 a technique was described by Doctor Chen Xin and colleagues which allowed for full catheterization of the canal even when a portion of the canal had been disrupted by prior surgery[5] This technique, “Relay Suture Guided Canaloplasty” (ReSGu Canaloplasty), is more challenging than primary canaloplasty. However, initial results are promising. One year after “Resgu” surgery average IOP had dropped from just over 32mmHg to less than 17mmHg (a reduction of nearly 50%)! Additionally, the average number of glaucoma medications required for IOP control dropped from just over three medications prior to rescue Canaloplasty to less than one medication after surgery.
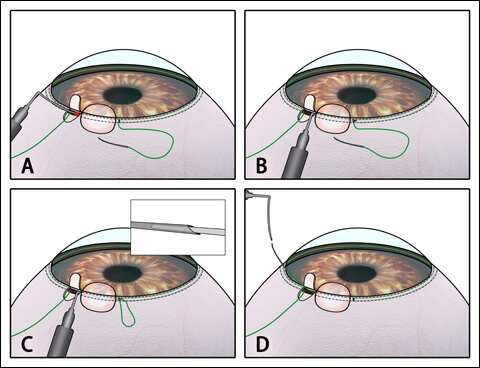
Relay suture with guidance of an illuminated trocar. A 10-0 polypropylene suture was placed within the remaining length of the canal (a). The illuminated trocar was guided to be inserted beneath the scleral flap containing the disrupted canal (b). The needle with placed 10-0 suture was attached to the trocar (c). The 10-0 suture was withdrawn, and the two ends of the suture loop were approximated (d). Source: Wang N
Given the recent development of this technique, longer term results are not available. Nonetheless, these early results are impressive. For those who are already experiencing the disappointment of failed glaucoma surgery it is somewhat comforting to realize that there is a lower-risk surgical option available: one that does not share the high risk of trabeculectomy or glaucoma drainage device placement.
References:
- Gedde SJ, Schiffman JC, Feuer WJ, et al. Treatment outcomes in the Tube Versus Trabeculectomy (TVT) study after five years of follow-up. Am J Ophthalmol. 2012;153:789-803.j
- Gedde SJ, Herndon LW, Brandt JD, et al. Postoperative Complications in the Tube Versus Trabeculectomy (TVT) Study During Five Years of Follow-up. Am J Ophthalmol. 2012 May;153(5):804-814.
- Law SK, Shih K, Tran DH, et al. Long-term outcomes of repeat vs initial trabeculectomy in open-angle glaucoma. Am J Ophthalmol. 2009;148:685-695.
- Bruisini P, Tosoni C. Canaloplasty after failed trabeculectomy: a possible option. J Glaucoma. 2014;23:33-34.
- Xin C, Chen X, Shi Y, Wang H, Wang N. Modified Canaloplasty: A New, Effective, and Safe Option for Glaucoma Patients With a Disrupted Schlemm Canal Wall. J Glaucoma. 2016;25:798-801.

David Richardson, MD
Medical Director, San Marino Eye
David Richardson, M.D. is recognized as one of the top cataract and glaucoma surgeons in the US and is among an elite group of glaucoma surgeons in the country performing the highly specialized canaloplasty procedure. Morever, Dr. Richardson is one of only a few surgeons in the greater Los Angeles area that performs MicroPulse P3™ "Cyclophotocoagulation" (MP3) glaucoma laser surgery. Dr. Richardson graduated Magna Cum Laude from the University of Southern California and earned his Medical Degree from Harvard Medical School. He completed his ophthalmology residency at the LAC+USC Medical Center/ Doheny Eye Institute. Dr. Richardson is also an Ambassador of Glaucoma Research Foundation.
Has Your Trabeculectomy Failed?
You may still be a candidate for Canaloplasty