Canaloplasty
Canaloplasty (pronounced Kah-NAL-oh-plas-tee) is an advanced minimally invasive glaucoma treatment. As glaucoma can cause a permanent loss of vision, this procedure can provide patients with glaucoma a “peace of mind” not possible with use of glaucoma drops alone. Canaloplasty can reduce eye pressure by nearly 40%, and most glaucoma patients who have had Canaloplasty can cut their glaucoma drops in half. In some cases, Canaloplasty can even eliminate the need for Glaucoma drops.
Canaloplasty can be done on its own or at the same time as cataract surgery (in which case it is called “PhacoCanaloplasty”). It is a “non-penetrating” glaucoma surgery which means it does not require creation of a hole in the eye (fistula) nor does it result in a “bleb” as required with the more traditional glaucoma surgery called trabeculectomy (“trab” for short).
Canaloplasty. Lower IOP. Fewer Drops.
Do you suffer from open angle glaucoma? Drops not working? Do you find it difficult to afford your medications or do they give you bothersome side effects? Canaloplasty is a newer, safer surgical treatment, which has been successfully helping many glaucoma patients worldwide control their eye pressure (IOP) – many, who after surgery, no longer need their eye drops!
How is Canaloplasty Performed?
Canaloplasty uses a micro-catheter to open the eye’s natural drainage system (“Schlemm’s canal”). This canal is then opened using a sterile, gel-like material (“viscoelastic”). The iTrack® micro-catheter is then removed while a suture is threaded through Schlemm’s canal. The suture is then tied down resulting in tension on the the inner wall of the canal – just as you might pull on the strings of a “hoodie” to close the hood over your face. The suture placed in the eye’s drainage canal can keep the canal stretched open for years. Once this canal is opened, the eye’s fluid can exit through a more natural process allowing the pressure in the eye to drop to a more normal level. Watch below video to see how Canaloplasty is performed.
What Are the Benefits of Canaloplasty?
- It uses the eye’s natural drainage system
- It is a “non-penetrating” procedure that does not create a permanent fistula in the wall of the eye
- It does not require a bleb (see why this is important What is the Big Deal About a Bleb, Anyway?
- Provides long-term reduction in IOP (see three year results below)
- Reduces the need for medications to keep the IOP controlled
- Is an option for patients that cannot tolerate medications because of side effects or cost (Drops are Difficult to Use – No Surprise Here)
- Is a good option for those patients with open angle glaucoma who are not yet ready for the more invasive traditional surgeries such as trabeculectomy or tube shunts
- Is safer than traditional glaucoma surgeries (Canaloplasty vs Trabeculectomy)
Is Canaloplasty Safe & Effective?
Yes, Canaloplasty Has Proven to Be Effective.
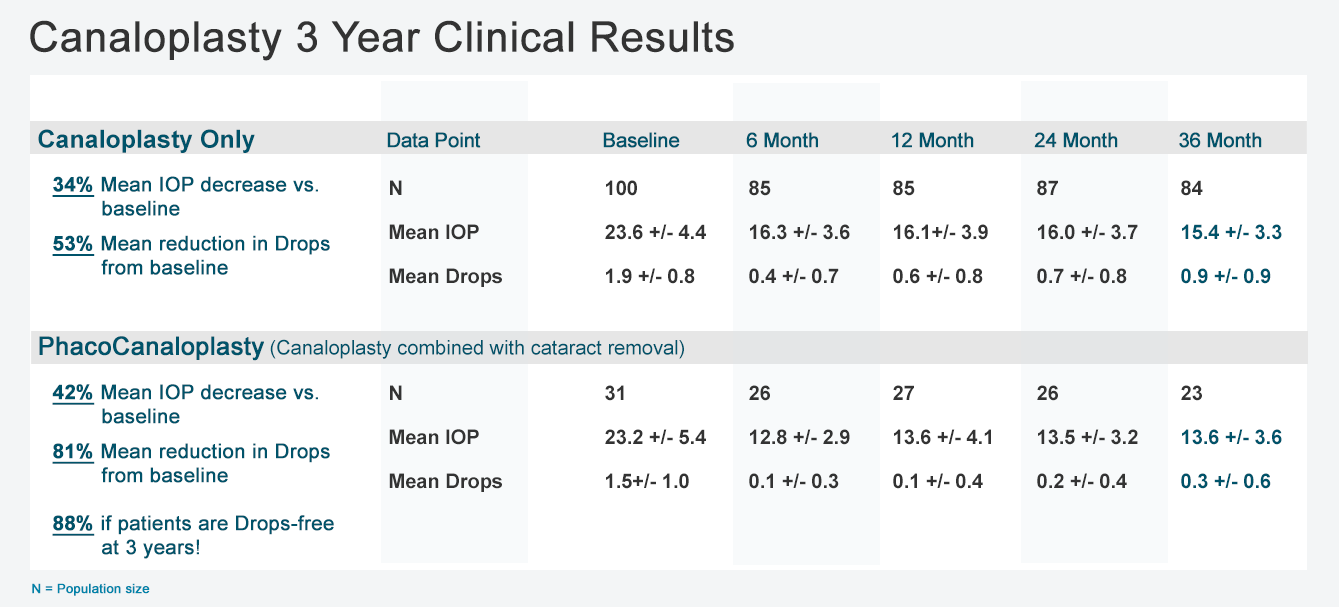
Canaloplasty showed very impressive results in the published 3 Year Clinical Study. Below are just some of the highlights. You may read the full article here Canaloplasty 3 Year Results Are In and They are Good!
- The number of medications required to keep the IOP under control was reduced by 53% … this sustained reduction in drops used means that the cost of canaloplasty could easily be paid just with the cost savings from using fewer medications to control IOP.
- The reduction in intraocular pressure (IOP) after canaloplasty was 34% – this was the lowest average IOP!
- The IOP in those patients who underwent Phacocanaloplasty™ was reduced by almost half (42%)!
- 88% of patients achieved IOP control without drops three years after canaloplasty!
Yes, Canaloplasty Has Been Proven to Be Effective.
Canaloplasty showed very impressive results in the published 3 Year Clinical Study. Below are just some of the highlights. You may read the full article here Canaloplasty 3 Year Results Are In and They are Good!
- The number of medications required to keep the IOP under control was reduced by 53% … this sustained reduction in drops used means that the cost of canaloplasty could easily be paid just with the cost savings from using fewer medications to control IOP.
- The reduction in intraocular pressure (IOP) after canaloplasty was 34% – this was the lowest average IOP!
- The IOP in those patients who underwent Phacocanaloplasty™ was reduced by almost half (42%)!
- 88% of patients achieved IOP control without drops three years after canaloplasty!
Yes. Canaloplasty Is Safe.
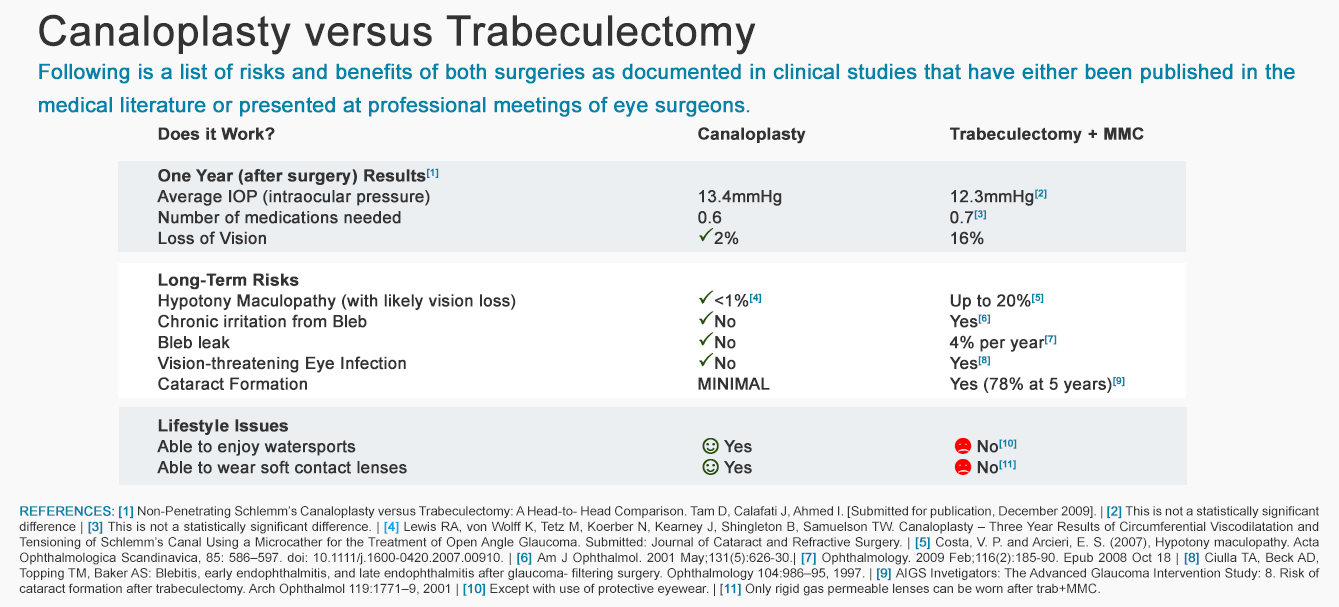
A study compared the results of Canaloplasty vs. trabeculectomy. Although there was no significant difference in the final intraocular pressures (IOPs) between the two surgeries (meaning both surgeries were equally good at lowering IOP), two differences were noted:
- Canaloplasty patients experienced fewer side effects and complications compared to those who had trabeculectomy; and
- the patients who had Canaloplasty had better vision than those patients who had trabeculectomy. For a more in-depth comparison, please read Canaloplasty vs Trabeculectomy.
Canaloplasty Frequently Asked Questions (F.A.Q.)
Have more questions? We have the answers. Check out our Canaloplasty Frequently Asked Questions for answers to over twenty of the most commonly asked questions about Canalopalsty
I’ve had Glaucoma Surgery. Can I have Canaloplasty?
If you have had either of the laser surgeries for open angle glaucoma (Argon Laser Trabeculoplasty or Selective Laser Trabeculoplasty), you may still be a candidate for Canaloplasty. It depends, however, on how much scarring there is from the laser surgery. Although your surgeon can visually inspect the area around Schelmm’s canal using a special contact lens (a technique called gonioscopy), s/he cannot tell if there has been permanent scarring of the canal itself. It may not be possible to fully catheterize the canal if there is dense scarring of the canal (called stenosis). In that case, your surgeon would not be able to stent the canal open with a suture, but would still inject a special gel (called a viscoelastic) into the partially opened canal. When the canal cannot be fully cannulated and the stent is not placed, this is called viscocanalostomy. Although not as effective as canaloplasty, it can still lower the IOP.
Will I be able to stop using Glaucoma drops after Canaloplasty?
Possibly. Remember that the primary objective of any glaucoma surgery (including Canaloplasty) is to lower your IOP into a safer range and protect you from further loss of vision. A secondary goal would be to reduce (or even eliminate) the use of glaucoma drops. Studies have shown Canaloplasty to be effective at achieving both of these goals. Not only do most people who undergo Canaloplasty have lower IOPs after surgery, but on average, they are able to stop just under two medications. What does “just under two” mean? Well, some people are able to stop one drop, some two, others none and some are even able to stop all of their drops. How many you will be able to stop if you have Canaloplasty cannot be predicted, though it’s likely that you will be able to stop at least one of them if you are on multiple drops.
Is Canaloplasty really safer than traditional Glaucoma suregery, Trabeculectomy?
Yes. A recent study compared one year results of Canaloplasty vs. trabeculectomy. Although there was no significant difference in the final intraocular pressures (IOPs) between the two surgeries (meaning both surgeries were equally good at lowering IOP), two differences were noted:
- Canaloplasty patients experienced fewer side effects and complications compared to those who had trabeculectomy; and
- The patients who had Canaloplasty had better vision than those patients who had trabeculectomy. For a more in-depth comparison, please read Canaloplasty versus Trabeculectomy.
I wear soft contact lenses. Can I continue to wear them after Canaloplasty?
Yes, but you may have to wait until the eye is healed from surgery. How soon you may restart use of contact lenses will be up to your surgeon. Additionally, it may be necessary to get fitted for new contact lenses after Canaloplasty as the surgery can sometimes change your refractive error. Contrast this with traditional glacuoma surgery (trabeculectomy). Because of the fragile nature of a bleb after trabeculectomy (and the risk of rupture and/or infection), once someone has had trabeculectomy surgery s/he cannot wear soft contact lenses after surgery for as long as the bleb is functioning. Hard contact lenses, however, are generally OK to wear even with trabeculectomy (though a refitting may be needed after surgery).
To view all FAQs, please download Canaloplasty Surgery FAQ eBook (Free)

Dr. David Richardson is among a select group of ophthalmologists in California offering Canaloplasty as a treatment option for his glaucoma patients. He has received numerous awards and is the personal eye surgeon for many of the most respected doctors in the San Gabriel valley. Dr. David Richardson tracks his Canaloplasty results and publishes them for everyone to see. View Canaloplasty Surgery Results.