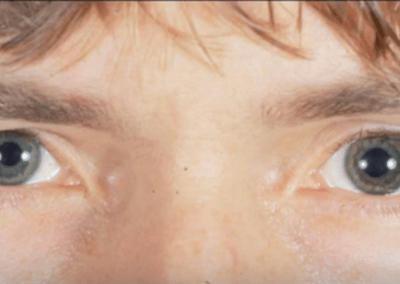
Glaucoma is a disease of old people. Or so you might think. And, you’d be more right than wrong. But there is a select group of younger adults who are at significant risk of developing glaucoma in their 20s or 30s. Could you be one of these individuals? How would you know? To find out, answer the following questions:
- Are you nearsighted (myopic)?
- Do you have a higher than average intelligence?
- Would you (or your friends or family) describe yourself as particularly “driven” or goal oriented?
- Would you describe your baseline sense of anxiety as more tense than relaxed?
If you answered “yes” to any of these questions you may be at risk for a condition called Pigment Dispersion Syndrome (PDS). This syndrome can result in damage to the optic nerve leading to a permanent loss of vision. When that happens the syndrome is called Pigment Dispersion Glaucoma (PDG). Unfortunately, if you had either of these syndromes you would have no way of knowing it yourself. You would just slowly and silently lose vision.
Both Pigment Dispersion Syndrome and Pigment Dispersion Glaucoma can, however, be detected by experienced ophthalmologists (eye surgeons) who are trained to look for the often subtle findings visible only at the examination microscope. When found, loss of vision from these syndromes can often be slowed, halted, or (if caught early enough) even prevented.
If you’re near-sighted (myopic), you have a particularly high risk of developing this condition.[1] Yet if the only eye doctor you’ve ever seen is the optometrist who prescribes your glasses or contact lenses, you may not have been adequately screened for Pigment Dispersion Syndrome. Indeed, even many ophthalmologists (“eye MDs”) are unaware of the earliest signs or subtle associations of this condition. As such, an examination by an ophthalmologist who treats a fair amount of glaucoma would likely provide the greatest chance of detecting these syndromes if present.
Photo Credit: Wallace L.M. Alward, M.D. | Frederick C. Blodi Chair • Department of Ophthalmology • University of Iowa Carver College of Medicine • Access URL: https://youtu.be/pPyo-vV4010
So what, exactly, is Pigment Dispersion Syndrome?
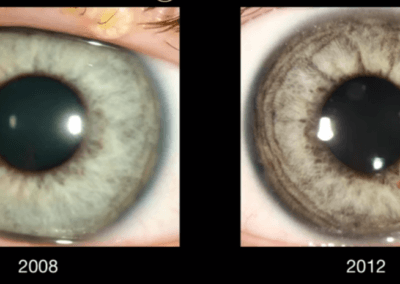
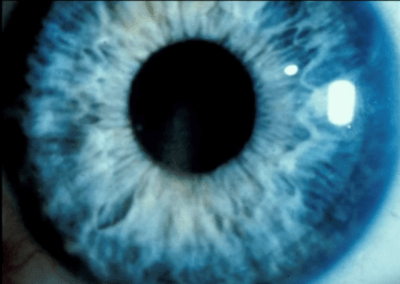
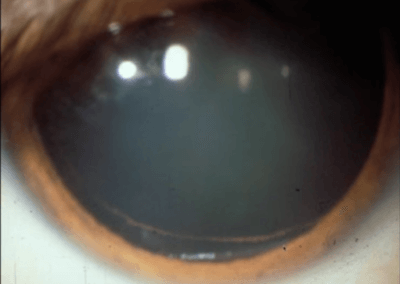
The back surface of the iris (colored part of the eye) is normally coated with pigment. In those with Pigment Dispersion Syndrome and Pigment Dispersion Glaucoma this pigment rubs off and floats around the front of the eye. Eventually, the pigment leaves the eye through the Trabecular Meshwork which is a grate-like structure and part of the eye’s natural drainage system. However, just as pouring too many coffee grounds down the kitchen sink can clog the drain, so does this pigment eventually clog the Trabecular Meshwork.
If the eye’s drainage system is clogged then pressure builds up inside the eye. This elevated intraocular pressure (IOP) eventually causes damage to the optic nerve (which sends the visual signal from the eye to the brain). A damaged optic nerve leads to permanent loss of vision. When this occurs the condition is called Pigment Dispersion Glaucoma.
Fortunately, if caught early, both Pigment Dispersion Syndrome and Pigment Dispersion Glaucoma can be effectively treated. Treatment may be in the form of eye drops or laser therapy.
Unfortunately, the eye drops that work best (Pilocarpine) are poorly tolerated among younger patients as this medication can be associated with headaches and blurred vision. Pilocarpine also increases the risk of retinal detachment.[2] Given that anyone who is significantly nearsighted is already at risk of retinal detachment, adding to that risk must be done with both great need and great caution. Also of concern is evidence that Pigment Dispersion Syndrome independently increases the risk of retinal detachment.[3]
Other eye drops that are commonly prescribed to treat glaucoma may also be used, though they may not be as effective as would Pilocarpine in the treatment of Pigment Dispersion Glaucoma. As such, it may be reasonable to consider laser therapy. To be most effective, two separate laser treatments may be necessary: Laser Trabeculoplasty and Laser Peripheral Iridotomy.
Laser Trabeculoplasty (LT), described in more detail here, directly treats the Trabecular Meshwork (TM) of the eye. When successful, this glaucoma laser treatment results in greater flow through the TM, lowering the intraocular pressure (IOP) which then protects the optic nerve. Unfortunately, this treatment may only last for months or years before the pigment once again clogs the eye’s drainage system and the IOP rises again.[4]
Laser Peripheral Iridotomy (LPI), creates a small hole in the iris. This allows fluid in the eye to move more freely from the front portion of the eye to the back. There is evidence that a pressure gradient may worsen the release of pigment from the iris surface. By reducing this pressure difference less pigment should rub off the iris. Lowering the rate of dispersion reduces the amount of clogging of the drainage system which over time decreases the eye pressure.
A Silver Lining in this Cloud of Pigment Dispersion
Fortunately, there is only so much pigment on the backside of the iris. Eventually, all the pigment that can be released will have been rubbed off. Once that happens, if the drainage system of the eye has not been irreversibly clogged, then the remaining pigment will over time flush through the system and the IOP will drop back into the normal range. However, any damage that has already been done to the optic nerve (as well as the associated loss of vision) will be permanent.
Summary
Pigment Dispersion Syndrome and Pigment Dispersion Glaucoma are syndromes that most commonly affect nearsighted (myopic), highly intelligent, driven, Type A, young adults.[5] There are generally no symptoms to alert the individual that s/he may be at risk of losing sight. Untreated, however, Pigment Dispersion Glaucoma can lead to irreversible loss of vision. Fortunately, an in-person examination by an experienced ophthalmologist can detect all but the earliest forms of these ocular syndromes. If detected early, treatment may even be able to prevent loss of vision.
If you answered “yes” to any of the questions at the beginning of this article, you may be at risk for developing loss of vision from Pigment Dispersion Glaucoma. Add “Research Ophthalmologists in my area” to your Getting Things Done® to-do list. If you happen to be in my area and would like to schedule an examination with me, you may request a consultation by calling the phone number or filling out the form here. My staff will work with you to find a mutually convenient date and time.
References
- Scheie HG, Cameron JD. Pigment dispersion syndrome: a clinical study. Br J Ophthalmol 1981; 65:264-269.
- Kraushar MF, Steinberg JA. Miotics and retinal detachment: upgrading the community standard. Surv Ophthalmol 1991; 35:311-316.
- Delaney WV. Equatorial lens pigmentation, myopia, and retinal detachment. Am J Ophthalmol 1975; 79:194-196.
- Ritch R, Liebmann JM, Robin AL, et al. Argon laser trabeculoplasty in pigmentary glaucoma. Ophthalmology 1993; 100:909-913.
- Personal communication with Dr. Robert Ritch, MD
Don’t delay getting checked for glaucoma.
Make an appointment with an eye doctor in your area now. If you live in the greater Los Angeles area and would like Dr. Richardson to evaluate your eyes for glaucoma call 626-289-7856 now. No referral required. Appointments are available, Tuesday through Saturday.

David Richardson, MD
Medical Director, San Marino Eye
David Richardson, M.D. is recognized as one of the top cataract and glaucoma surgeons in the US and is among an elite group of glaucoma surgeons in the country performing the highly specialized canaloplasty procedure. Morever, Dr. Richardson is one of only a few surgeons in the greater Los Angeles area that performs MicroPulse P3™ "Cyclophotocoagulation" (MP3) glaucoma laser surgery. Dr. Richardson graduated Magna Cum Laude from the University of Southern California and earned his Medical Degree from Harvard Medical School. He completed his ophthalmology residency at the LAC+USC Medical Center/ Doheny Eye Institute. Dr. Richardson is also an Ambassador of Glaucoma Research Foundation.