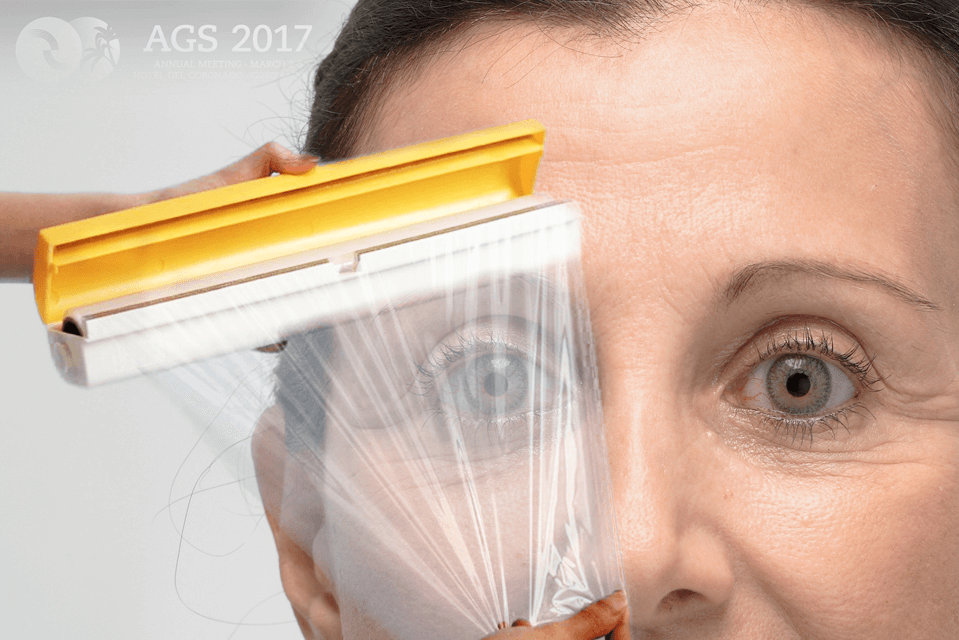
What Does Cellophane Have to Do with Glaucoma?
Glaucoma is an eye disease commonly associated with aging. The development of “floaters” in one’s visual field is also more likely as we get older. A portion of those with floaters will later develop a clear membrane on the retina which closely resembles SaranTM Wrap. This condition is commonly referred to by the name Cellophane Maculopathy or Epiretinal Membrane.
Although we are all more likely to develop glaucoma and cellophane maculopathy as we age, not all of us will. Why do some of us develop these conditions while others do not? Cellophane maculopathy is known to be associated with growth of a particular type of cell call glial cells. These cells respond to inflammation. Recent evidence suggests that glial cells may also be activated in those with glaucoma. So, could cellophane maculopathy and glaucoma be related?
 Dr. Luna Xu and colleagues addressed this issue at the recent American Glaucoma Society (AGS) 2017 Annual Meeting in Coronado, CA in their poster, “Is Macular Pucker Associated with More Severe Glaucoma?” They inspected the charts of patients who had glaucoma in both eyes and needed surgery to treat cellophane maculopathy in only one eye (indicating that the macular condition was severe enough to limit vision).
Dr. Luna Xu and colleagues addressed this issue at the recent American Glaucoma Society (AGS) 2017 Annual Meeting in Coronado, CA in their poster, “Is Macular Pucker Associated with More Severe Glaucoma?” They inspected the charts of patients who had glaucoma in both eyes and needed surgery to treat cellophane maculopathy in only one eye (indicating that the macular condition was severe enough to limit vision).
What they found was that the eyes which required surgery to treat cellophane maculopathy had evidence of worse glaucoma than the fellow eyes without the epiretinal membrane. This was true for both cup-to-disc and Visual Field Index measurements.
Although this study was quite small (only eight patients met the inclusion criteria), it provides further support that glaucoma is not only a disease of eye pressure (IOP). Indeed, the results of this study suggest that inflammation may be associated with worsening glaucoma. There is mounting evidence suggesting inflammation plays a role in all diseases, even aging itself. It seems glaucoma is no exception.
In the meantime, I will continue to tell my patients with glaucoma that “What’s good for the body (healthy diet and exercise) is good for the optic nerve”.
What can be done with this information? For one, studies could be funded with the goal of developing anti-inflammatory treatments of glaucoma. It’s even possible that lifestyle modifications such as avoiding “pro-inflammatory” foods could be of benefit to those with glaucoma. Whether these assumptions pan out, however, will require years of research to prove. In the meantime, I will continue to tell my patients with glaucoma that “What’s good for the body (healthy diet and exercise) is good for the optic nerve”.
Reference:
- Vargas JL, Belforte N, Di Polo A. The glial cell modulator ibudilast attenuates neuroinflammation and enhances retinal ganglion cell viability in glaucoma through protein kinase A signaling. Neurobiology of Disease 2016;93:156-71.
Don’t delay getting checked for glaucoma
Make an appointment with an eye doctor in your area now. If you live in the greater Los Angeles area and would like Dr. David Richardson to evaluate your eyes for glaucoma call 626-289-7856 now. Appointments are available Tuesday through Saturday.

David Richardson, MD
Medical Director, San Marino Eye
David Richardson, M.D. is recognized as one of the top cataract and glaucoma surgeons in the US and is among an elite group of glaucoma surgeons in the country performing the highly specialized canaloplasty procedure. Morever, Dr. Richardson is one of only a few surgeons in the greater Los Angeles area that performs MicroPulse P3™ "Cyclophotocoagulation" (MP3) glaucoma laser surgery. Dr. Richardson graduated Magna Cum Laude from the University of Southern California and earned his Medical Degree from Harvard Medical School. He completed his ophthalmology residency at the LAC+USC Medical Center/ Doheny Eye Institute. Dr. Richardson is also an Ambassador of Glaucoma Research Foundation.


