Glaucoma Cell Biology Laboratory of the Iowa Glaucoma Center at the University of Iowa Carver College of Medicine.n| Source: myweb.uiowa.edu/kuehnm
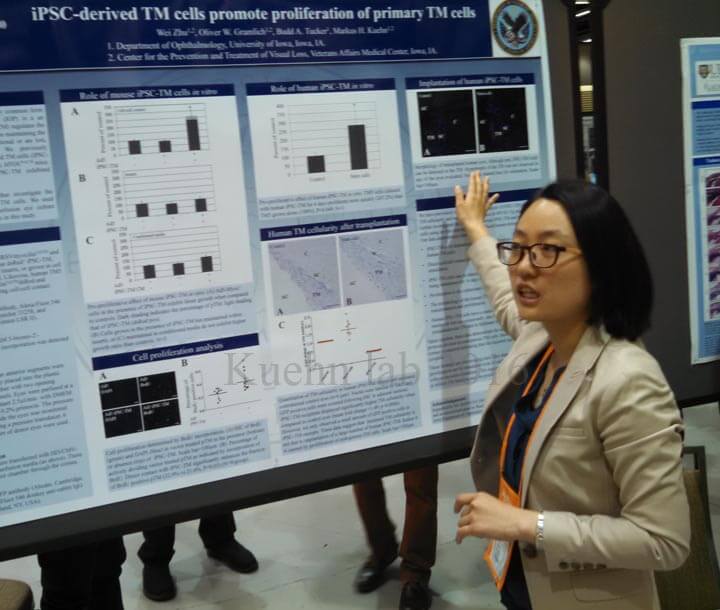
Dr. Markus Kuehn presented a fascinating talk on the “Role of Stem Cells for Trabecular Meshwork Regenerative Medicine in Glaucoma” at the recent American Glaucoma Society (AGS) 2017 Annual Meeting in San Diego, CA (March 2-5).
Open angle glaucoma is thought to be largely due to a poorly working trabecular meshwork (TM). The trabecular meshwork is essentially the drainage grate of the eye. It makes sense, then, that if the grate is “clogged” and fluid cannot leave the eye fast enough that pressure (IOP) would build up in the eye causing damage to the optic nerve.
There are cells in the trabecular meshwork that actively move fluid from the anterior chamber (inside of the eye) to Schlemm’s canal (the drainage canal). Elevated IOP is associated with lower cell density in the trabecular meshwork. It stands to reason that if the number of these cells could be increased then the trabecular meshwork might be better able to move fluid out of the eye. This would result in a lower IOP.
The research presented data regarding induced pluripotent stem cells (iPSC-TM). These stem cells are taken from the individual (not a fetus), are easily obtained, and are patient-specific. As such, there are no ethical issues nor is there a significant concern about the body rejecting the cells as “foreign”.
These stem cells are taken from the individual (not a fetus), are easily obtained, and are patient-specific.
In mice transplanted with iPSC-TM the aqueous humor outflow facility (drainage of fluid out of the eye) improved within two months of surgery. This was associated with increased cellular density of the trabecular meshwork, IOP control, and protection of the retinal ganglion cells (usually damaged by elevated IOP).
In mice transplanted with iPSC-TM the aqueous humor outflow facility (drainage of fluid out of the eye) improved within two months of surgery.
Surprisingly, not all of the new trabecular meshwork cells were derived from the stem cells. It seems that the stem cells are able to “encourage” the cells that are already there to divide into new functioning cells.
It’s really something to see how far stem cell research has come in such a short amount of time. We owe Dr. Kuehn and others who are actively pursuing this research a debt of gratitude for bringing us closer to a cure for glaucoma.

David Richardson, MD
Medical Director, San Marino Eye
David Richardson, M.D. is recognized as one of the top cataract and glaucoma surgeons in the US and is among an elite group of glaucoma surgeons in the country performing the highly specialized canaloplasty procedure. Morever, Dr. Richardson is one of only a few surgeons in the greater Los Angeles area that performs MicroPulse P3™ "Cyclophotocoagulation" (MP3) glaucoma laser surgery. Dr. Richardson graduated Magna Cum Laude from the University of Southern California and earned his Medical Degree from Harvard Medical School. He completed his ophthalmology residency at the LAC+USC Medical Center/ Doheny Eye Institute. Dr. Richardson is also an Ambassador of Glaucoma Research Foundation.