How is Glaucoma Treated?
It’s been mentioned already that glaucoma is likely a disease with many causes. As the oldest understanding of this disease relates to elevated intraocular pressure (IOP) it should come as no surprise that most available glaucoma treatments are directed at lowering IOP.
For many decades, it has been believed that the “normal” eye pressure was considered to be between 8-21 mmHg. The goal of treatment, therefore, used to be simply to get one’s eye pressure (IOP) into this range. We now know that this was a gross oversimplification. Why? Because there are people who are able to tolerate IOPs well above 21mmHg for years without showing any signs of glaucoma. Others, however, develop progressive loss of vision even with IOPs well below 21mmHg. How can this be? Well, just as some people are able to lift a 100lb weight without straining a muscle whereas others might be seriously hurt by trying, each individual’s optic nerve is able to tolerate only so much pressure. How much an individual nerve can tolerate, exactly, is the mystery that must be solved by your doctor.
So, if we can’t just say, “Under 21mmHg is OK,” then how do we know what IOP is “OK” for an individual? In general, once treatment is started, the initial goal of therapy is to decrease the IOP by 20% to 30% below the pre-treatment IOP measurement.
Your doctor may consider your glaucoma stage, IOP range prior to treatment, age, life expectancy, status of the fellow eye, other disease history, race, and or family history when choosing an IOP lowering goal. As you can see, there can be a lot that goes into determining what IOP is OK for you. This IOP is called the “target IOP” and may be very different for you than for others you know who also have glaucoma.
To further complicate matters, the target IOP is not an absolute, or unchanging, value. Just as there are some patients with glaucoma that progresses even when the “target IOP” has been reached, there are also those with glaucoma that show no progression even though the target has not been achieved. Additionally, as glaucoma progresses the optic nerve becomes more sensitive to IOP requiring that the IOP be lowered further still. Because of these factors, the target IOP must be periodically re-evaluated and revised by your doctor.
It’s not just the magnitude of IOP that matters. There is also evidence that IOP fluctuation can be damaging to the optic nerve. In other words, it may not be good enough to just lower the IOP. It may also be necessary to reduce the range of IOP fluctuation in order to achieve optimal protection of the optic nerve.
IOP Lowering Therapies
Since the 19th century the mainstay of glaucoma treatment has been to lower the eye pressure. This has been achieved through both medical and surgical means:

Medical Therapies
As far back as 1876 physostigmine (an extract of the Calabar bean) was used to treat glaucoma. Development of medical therapies for glaucoma has been slow with only five classes of medications commonly prescribed today.
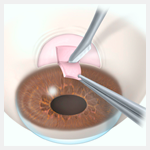
Surgical Therapies
IOP lowering surgeries have been around since the mid-nineteenth century. Because of the many risks of older glaucoma surgeries this option has generally been withheld until the late stages of glaucoma.
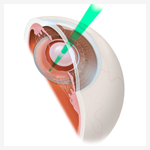
Laser Therapies
The use of laser to treat glaucoma began in the 1970s. Although the newest form of glaucoma treatment, it is one of the safest.
Therapies not Directly Related to Intraocular Pressure
At the present time all FDA approved glaucoma treatments aim to lower IOP. However, modern research has discovered a number of mechanisms other than elevated IOP that may contribute to loss of vision from glaucoma. A few of these mechanisms include:
- Reducing inflammation
- Limiting oxidative damage
- Neuroprotection
- Improving the blood supply to the optic nerve
References
- Singh K, Shrivastava A. Intraocular pressure fluctuations: how much do they matter? Curr Opin Ophthalmol. 2009;20:84-7.
- Sultan MB, Mansberger SL, Lee PP. Understanding the importance of IOP variables in glaucoma: a systematic review. Surv Ophthalmol. 2009;54:643-62.
Don’t delay getting checked for glaucoma.
Make an appointment with an eye doctor in your area now. If you live in the greater Los Angeles area and would like Dr. Richardson to evaluate your eyes for glaucoma call 626-289-7856 now. No referral required. Appointments are available, Tuesday through Saturday.


