Vital Signs
In medicine “vital signs” are those measurements considered critical to the health of an individual. Common vital signs include temperature, heart rate, breathing rate, and blood pressure. But there are also vital signs of the eye. Visual acuity (e.g., “20/20”) and intraocular pressure (IOP) are two such measurements. For the last twenty years, those with ocular hypertension or glaucoma have had a third vital sign: central corneal thickness (CCT). Corneal thickness can be used (among other things) to estimate how likely someone may be to develop glaucoma. However, a newly discovered measurement has proven to be even more valuable than CCT. This new measurement is called Corneal Hysteresis (“CH”).
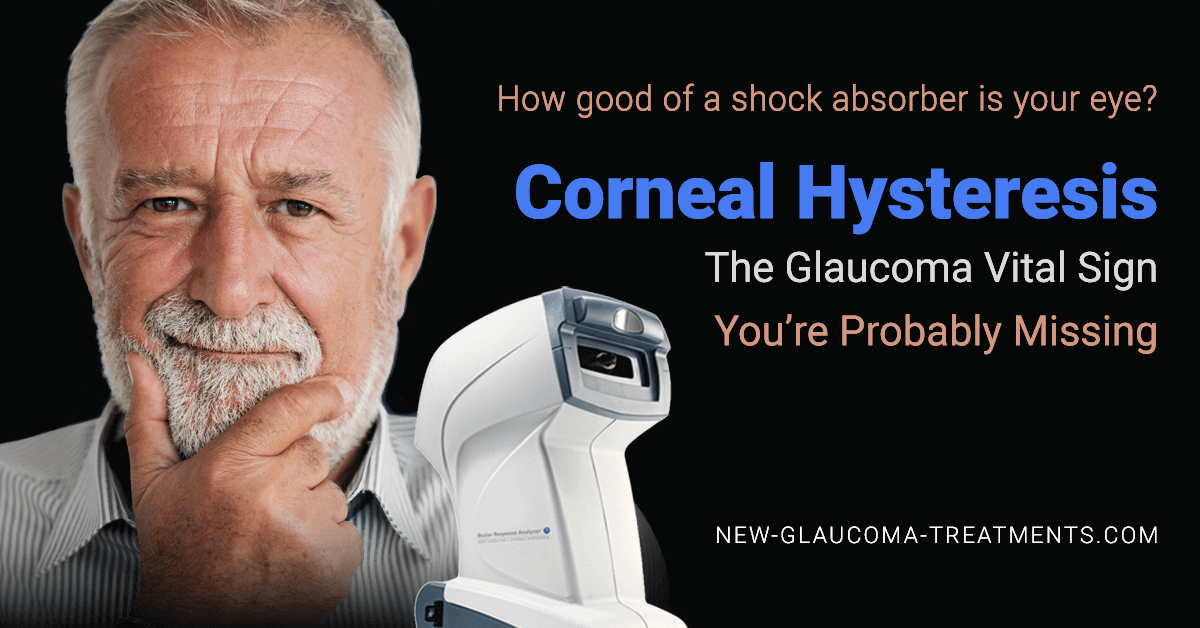
What is Corneal Hysteresis?
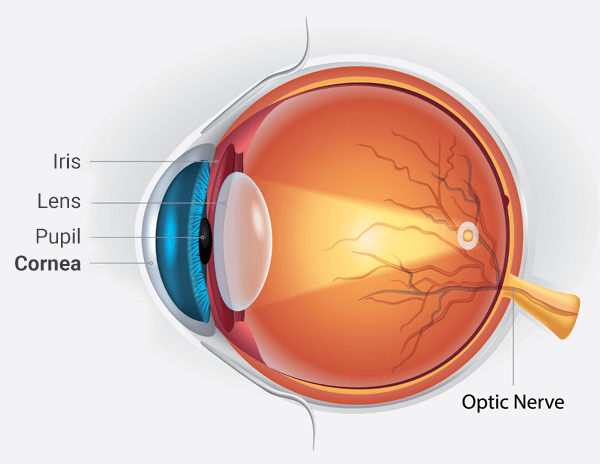
The cornea is the clear (transparent) surface at the front of the eye which focuses light onto the lens inside the eye. It can be thought of as a half-millimeter thick soft contact lens. Like a soft contact lens, it is deformable (“bendy”). Many biological tissues that can be flexed or bent without permanent damage can be described as “viscoelastic”. Viscoelastic tissues absorb some of the force used to deform them like the suspension strut in your car or truck works to absorb the impact of a pothole.
Corneal hysteresis essentially measures the “shock-absorbing” ability of the cornea. The higher the corneal hysteresis, the greater the shock-absorbing capacity of the cornea (and perhaps the eye).
Why Should I Care?
It turns out that a low corneal hysteresis may be predictive of the presence of glaucoma and its progression (worsening over time). In particular, a low corneal hysteresis:
“A low corneal hysteresis can help predict who might develop glaucoma[1]”
- Increases the risk of further damage to the optic nerve[3]
- Increases the risk of progressive visual field loss[4]
- May help in predicting which patients with normal tension glaucoma are more likely to lose vision[5]
- May predict who will respond to certain IOP lowering therapies. For example, a low corneal hysteresis is associated with a greater reduction of IOP after treatment with a class of IOP lowering eye drops known as the prostaglandin analogs (latanoprost being the most common)[6]. This also appears to be the case with certain surgical treatments such as selective laser trabeculoplasty (SLT)[7].
What might be the reason for these associations?
It’s thought that corneal hysteresis may be similar to whole eye hysteresis. In other words, a low corneal hysteresis may indicate that not only is the cornea unable to adequately deal with changes in force, but the entire eye may be subject to damage from repetitive shocks. The eye suffers from a lot of physical abuse during the day as it is rapidly moved inside the orbit and it is squeezed by the eyelids during blinking.
Both elevated IOP and fluctuations in IOP can result in damage to the optic nerve. We kind of understand why elevated IOP is bad, but why fluctuating IOP is a risk for glaucoma is less well understood. Hysteresis may provide one answer (if not the answer) to this question. After all, if an eye has a limited ability to absorb shock then it makes sense that fluctuating IOP (essentially mini-shocks) would increase the likelihood of damage to the eye.
I already know my Corneal Thickness measurement. How is CH different?
Low central corneal thickness (CCT) measurements are also known to be associated with glaucoma risk. However, corneal hysteresis is more strongly associated with glaucoma presence, risk of progression[8], and effectiveness of glaucoma treatments than central corneal thickness. Thus, if you could choose only one corneal measurement, you would be wise to choose Corneal Hysteresis over central corneal thickness.
Who Needs a Corneal Hysteresis measurement?
If you fit into one of the following groups you could benefit from knowing your corneal hysteresis:
- You have someone in your family with glaucoma
- You have diabetes (which can increase your risk of developing glaucoma)
- You are nearsighted (which can increase your risk of developing glaucoma)
- You have elevated eye pressure (“ocular hypertension”)
- You’ve been told that you are a “glaucoma suspect”
- Your doctor is considering placing you on glaucoma medications
- You’ve just started a new glaucoma medication
- You are considering the option of glaucoma surgery
- You have just healed from glaucoma surgery
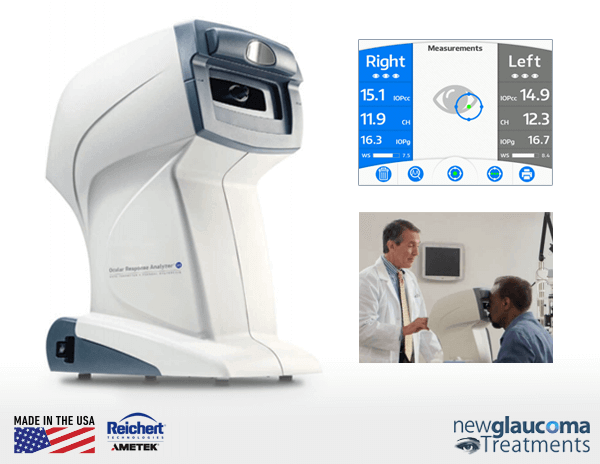
How Is Corneal Hysteresis Measured?
Corneal Hysteresis (“CH”) measures a biomechanical property of the cornea. That’s just a fancy way of saying, “let’s do something to the cornea and see what happens”. In the case of the cornea, it’s pushed by a stream of air until just after its surface flattens enough to reflect light. The cornea then “relaxes” (yeah, that’s what I’d do if I had just been pummelled by a jet of air) back into its normal shape. On its way back the surface transitions through the light reflecting phase again. The pressure of air

The ORA’s sensor consists of an infrared light emitter, a light detector, and a pneumatic tonometer.
applied to the cornea is also measured throughout the movement of the cornea. The difference between the pressure applied at the two light-reflecting moments is the corneal hysteresis measurement.
So, the measurement of corneal hysteresis is essentially an “air puff” test similar to the way many optometrists measure intraocular pressure (IOP). However, most “air puff” tonometers (IOP measuring devices) do not measure corneal hysteresis. Only the Reichert Ocular Response Analyzer (ORA) is capable of and FDA approved to perform measurement of corneal hysteresis.
Air puff tonometers have gotten a bad rap in the past (well, kind of deservedly so) as the air puff was strong and unpleasant for many taking the test. Additionally, they were not very accurate or reliable. However, they benefited from the fact that no anesthesia was necessary to obtain the measurement. The Reichert ORA “air puff” is much gentler than that used by prior technologies, though the air puff can be somewhat surprising at first. As for clinical value, there is evidence that the IOP measurement obtained from the Reichert ORA (the “IOPcc”) may be even better than the commonly accepted “gold standard”, Goldmann applanation tonometry (“GAT”)[9].
What is a Normal Corneal Hysteresis Number?
Similar to intraocular pressure (IOP) measurements, corneal hysteresis is measured in millimeters of mercury (mmHg) and can be thought of as the corneal hysteresis “number”, or “CH number”.
Corneal hysteresis has a range of normal values. Asians average around 11mmHg; Caucasians, 10; Hispanics, 9½; African Americans between 8½ and 9. This distribution has not been validated, however, so it’s likely that any measurement over 8.5mmHg could be considered “normal”.
Interestingly, corneal hysteresis is not a static (or “fixed”) number. It can change with time. Indeed, corneal hysteresis may increase in eyes after IOP-lowering interventions are implemented.
Should I Worry if my Corneal Hysteresis Number is Low?
A low CH number on its own doesn’t mean that glaucoma is inevitable. However, the combination of a low corneal hysteresis and a high IOP is predictive of loss of vision over time. As such, this combination may suggest to your eye doctor that more aggressive lowering of the IOP is needed.
How Often Should I get my Corneal Hysteresis Number?
Corneal Hysteresis is a dynamic value, meaning that it can change over time. Although it does not change as rapidly or as often as IOP, effective treatment of IOP can increase corneal hysteresis. As such, it is a good idea to repeat the corneal hysteresis measurement after any change in glaucoma therapy (such as eye drops, laser, or other surgery).
How can I get my Corneal Hysteresis Number?
Unfortunately, as the technology to measure corneal hysteresis has only been around since 2005[10] very few doctor’s offices can perform this test. Some academic centers do, but not all. Although nowhere near as expensive as most modern diagnostic eye equipment, the equipment used to obtain the corneal hysteresis measurement is substantially more expensive than most tonometers (devices used to measure IOP). Then again, it’s providing a lot more information as well.
If you have glaucoma (or are at significant risk of developing glaucoma) you may wish to call around to see who in your area is providing this service. Insurance may cover or reimburse you for a portion of the testing fee.
I have decided that the measurement of corneal hysteresis is important enough to provide to my patients with glaucoma or who might be at risk for glaucoma. This includes anyone with elevated IOP, suspicious appearing optic nerves, family history of glaucoma, history of diabetes, history of myopia (“nearsighted”). If you fall into one of these (or other glaucoma risks) categories and have not yet obtained a measurement of corneal hysteresis, I encourage you to make an appointment with a doctor in your area who has this important technology.

David Richardson, MD
Medical Director, San Marino Eye
David Richardson, M.D. is recognized as one of the top cataract and glaucoma surgeons in the US and is among an elite group of glaucoma surgeons in the country performing the highly specialized canaloplasty procedure. Morever, Dr. Richardson is one of only a few surgeons in the greater Los Angeles area that performs MicroPulse P3™ "Cyclophotocoagulation" (MP3) glaucoma laser surgery. Dr. Richardson graduated Magna Cum Laude from the University of Southern California and earned his Medical Degree from Harvard Medical School. He completed his ophthalmology residency at the LAC+USC Medical Center/ Doheny Eye Institute. Dr. Richardson is also an Ambassador of Glaucoma Research Foundation.
References:
[1] A Prospective Longitudinal Study to Investigate Corneal Hysteresis as a Risk Factor for Predicting Development of Glaucoma. AJOPHT 10365 – in press. Feilin Zhu , Alberto DinizFilho, Linda M. Zangwill , Felipe A. Medeiros
[2] Congdon NG, Broman AT, Bandeen-Roche K, Grover D, Quigley HA. Central corneal thickness and corneal hysteresis associated with glaucoma damage. Am J Ophthalmol. 2006 May;141(5):868-75.
[3] Zhang C, Tatham AJ, Abe RY, Diniz-Filho A, Zangwill LM, Weinreb RN, Medeiros FA. Corneal Hysteresis and Progressive Retinal Nerve Fiber Layer Loss in Glaucoma. Am J Ophthalmol. 2016 Jun;166:29-36
[4] Medeiros FA, Meira-Freitas D, Lisboa R, Kuang TM, Zangwill LM, Weinreb RN. Corneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal study. Ophthalmology. 2013 Aug;120(8):1533-40.
[5] Park JH, Jun RM, Choi KR. Significance of corneal biomechanical properties in patients with progressive normal-tension glaucoma. Br J Ophthalmol. 2015 Jun;99(6):746-51.
[6] Agarwal DR, Ehrlich JR, Shimmyo M, Radcliffe NM. The relationship between corneal hysteresis and the magnitude of intraocular pressure reduction with topical prostaglandin therapy. Br J Ophthalmol. 2012 Feb;96(2):254-7.
[7] Hirneiß C, Sekura K, Brandlhuber U, Kampik A, Kernt M. Corneal biomechanics predict the outcome of selective laser trabeculoplasty in medically uncontrolled glaucoma.Graefes Arch Clin Exp Ophthalmol. 2013 Oct;251(10):2383-8.
[8] Park Et. Al Br J Ophthalmol. 2015 Jan 2. pii: bjophthalmol-2014-305962. doi: 10.1136/bjophthalmol-2014-305962.
[9] Goldmann applanation tonometry compared with corneal-compensated intraocular pressure in the evaluation of primary open-angle Glaucoma. Joshua R Ehrlich, Nathan M Radcliffe, and Mitsugu Shimmyo. BMC Ophthalmology 2012, 12:52
[10] Luce DA. Determining in vivo biomechanical properties of the cornea with an ocular response analyzer. J Cataract Refract Surg. 2005;31(1):156–162
Related Articles:
- EYEMATE Intraocular Pressure Sensor Implant Receives CE mark
- Association Between Rates of Glaucoma Visual Field Progression and Intraocular Pressure (IOP) Measurements Obtained by Different Tonometers
- The SENSIMED Triggerfish® Sensor Device
- IOP Monitoring Implant – A Glaucoma Surveillance System
- Intraocular Pressure (IOP) Monitoring
- Automated Contact Lenses To Revolutionize Glaucoma Treatment In The US Soon